Coronary artery disease can lead to various dangerous complications if not detected and treated early. The mortality rate associated with this condition is not insignificant, and the prevalence of the disease is on the rise. Therefore, understanding the causes of atherosclerosis is crucial.
1. What is Coronary Artery Disease?
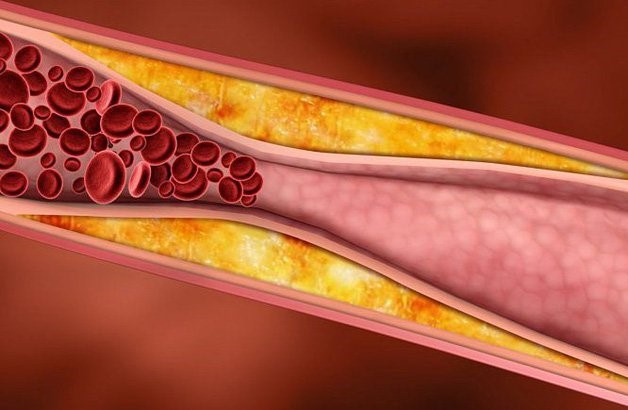
Arteries play a vital role in the body’s functions by transporting blood to nourish the heart and other organs. Over time, substances such as calcium, fats, or cholesterol accumulate in the arteries, forming atherosclerosis plaques.
Coronary artery disease occurs when the coronary arteries become stiff and narrowed due to the impact of atherosclerotic plaques, restricting blood flow and causing insufficient blood supply to organs. Particularly when it occurs in the arteries supplying the heart, it is referred to as coronary artery disease.
Coronary artery disease can occur silently for many years
When the coronary arteries are narrowed, localized blood deficiency occurs, leading to potential complications such as angina, myocardial infarction (heart attack), and heart failure. Patients may experience fatigue, shortness of breath, ankle swelling, and reduced urine output.
2. Causes Leading to Coronary Artery Disease
According to medical studies and evaluations, the primary causes of coronary artery disease include:
– Unhealthy dietary habits: Excessive consumption of saturated fats, animal fats, and metabolized fats (found in pastries, red meat, and processed foods) contributes to elevated cholesterol and the formation of lipid deposits in the artery walls.
– Obesity, overweight, or large waist circumference: Indicative of metabolic disorders, these conditions increase the risk of atherosclerosis by disrupting metabolism.
– Lack of physical activity: Insufficient exercise leads to an increase in blood lipids. Regular physical activity helps raise HDL-cholesterol levels.
– Excessive smoking habits: Smoking damages blood vessel walls, reduces HDL-cholesterol, and promotes the accumulation of LDL-cholesterol, contributing to atherosclerotic plaque formation.
– Aging: With increased age, metabolic changes and increased lipid retention in the blood vessels occur. Additionally, age-related elasticity changes in the arterial walls contribute to the development of atherosclerosis.
– Pre-existing conditions like diabetes, kidney disorders, and hypothyroidism: Chronic metabolic disorders significantly affect lipid metabolism, increasing the risk of atherosclerosis.
– Hypertension: Elevated blood pressure damages the inner lining of arteries, creating conditions for lipoprotein molecules to adhere and form atherosclerotic plaques.

Obesity can increase the risk of atherosclerosis
3. Complications and Treatment of Atherosclerosis
3.1. Complications of Coronary Artery Disease
Accumulation of atherosclerotic plaques has the potential to lead to dangerous complications:
– Thickening and narrowing of the arteries limit blood flow. Initially, there may be no significant symptoms.
– When the arteries are severely obstructed, stable angina may occur. This is characterized by chest pain during exertion, relieved by rest. Although not a heart attack, it serves as a warning sign requiring prompt treatment.
If an atherosclerotic plaque ruptures and a blood clot forms in the coronary artery, two scenarios may unfold:
– The blood clot may not completely block the artery, gradually dissolving without causing a heart attack.
– The blood clot may fully obstruct the coronary artery, leading to oxygen and nutrient deprivation in the heart muscle, causing irreversible damage to heart function.
3.2. Treatment of Coronary Artery Disease
The primary goals of treating coronary artery disease are to:
– Slow down or prevent the accumulation of plaques inside the coronary arteries.
– Significantly improve painful symptoms for patients.
– Prevent complications such as blood clot formation, arterial blockage, and heart failure.
– Enhance blood flow by expanding the artery lumen, minimizing internal blockages.
– Commonly applied methods include maintaining a healthy lifestyle, medication use, and various surgical procedures.

Regular daily exercise helps slow down the process of atherosclerosis
Adopting a healthy and scientifically balanced lifestyle is crucial for controlling the disease. Patients should:
– Quit smoking: Smoke is a major contributor to arterial damage and reduces blood oxygen levels.
– Adjust their diet: Increase fiber intake, consume healthy fats, and limit salt and sugar in daily meals. Avoid foods high in bad cholesterol, such as processed and fried foods.
– Manage stress and negative thoughts: Stress can increase blood pressure, a direct adversary to the disease. Effective stress management helps maintain stable blood pressure.
– Engage in regular exercise and physical activities.
Several types of medications may be prescribed to control the disease:
– Medications to control heart rate and blood pressure.
– Medications to lower LDL-cholesterol levels in the blood.
– Antiplatelet agents to minimize blood clot formation.
– In severe cases, surgical interventions such as stent placement or coronary artery bypass grafting may be necessary.
Early diagnosis and treatment enable patients to maintain a healthy life. However, vigilance is crucial due to the potential hidden risks of arterial blockage and heart attacks associated with this condition.








