Fatty liver disease, also known as hepatic steatosis, progresses through three distinct stages, each with unique characteristics and levels of risk. Recognizing the stages of fatty liver disease is essential for timely diagnosis and treatment, especially given the disease’s potential to escalate from mild to life-threatening. This article discusses each stage of fatty liver disease, symptoms, possible complications, and treatment recommendations for each phase.
1. Key Characteristics Across the Stages of Fatty Liver Disease
1.1 Stage 1: Early-Stage Fatty Liver Disease
In the initial stage of fatty liver disease, fat deposits account for roughly 5-10% of the liver’s total weight. This stage is often the least dangerous and, if detected early, can be managed and even reversed through lifestyle adjustments. Symptoms are typically subtle and may include mild fatigue or a general sense of discomfort, but many individuals remain asymptomatic. Routine health check-ups play a significant role in identifying fatty liver disease at this early stage.
1.2 Stage 2: Progression of Fatty Liver Disease
The second stage of fatty liver disease is marked by fat accumulation covering 10-25% of the liver. Fat begins to infiltrate the liver tissue and diaphragm, leading to a reduction in liver function. At this stage, symptoms become more noticeable, including reduced appetite, abdominal bloating, nausea, and unexplained fatigue. Diagnostic imaging often shows fatty tissue within liver cells, indicating a more advanced level of hepatic steatosis. Without intervention, the disease can rapidly progress, raising the risk of severe complications.
1.3 Stage 3: Advanced Fatty Liver Disease
In the final and most severe stage of fatty liver disease, fat accounts for 25-30% or more of the liver’s weight. This stage poses significant health risks as liver cells experience severe damage, and liver function begins to deteriorate markedly. Common symptoms include pain in the upper right abdomen, jaundice (yellowing of the skin and eyes), vascular lesions, persistent fatigue, and weight loss. The advanced stage of fatty liver disease requires intensive medical attention to prevent life-threatening outcomes such as liver failure.
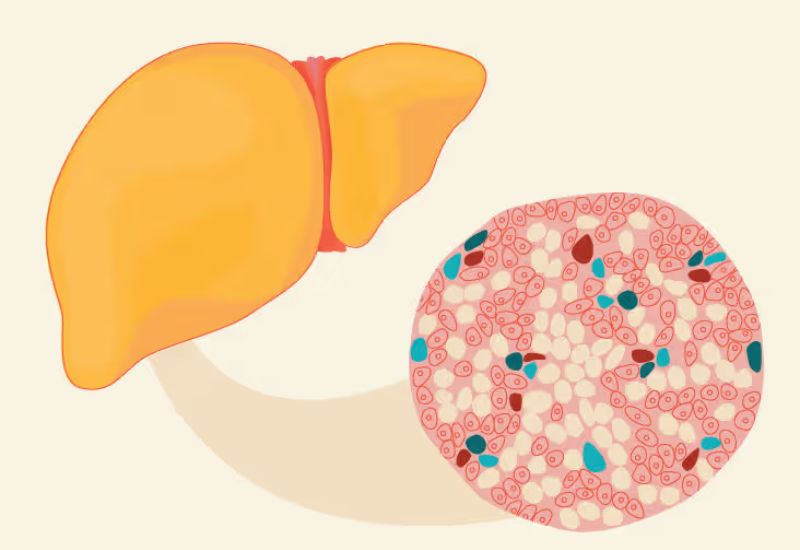
Fatty liver disease is categorized into three stages based on the level of fat accumulation in the liver.
2. Recognizing Symptoms Across the Stages of Fatty Liver Disease
2.1 Early Stage Symptoms
Mild and often asymptomatic, early-stage fatty liver disease may go unnoticed by many. Symptoms, if present, include general fatigue and occasional loss of appetite, both of which can be easily overlooked. Since symptoms are minimal, the disease is frequently detected only during routine medical exams.
2.2 Symptoms in Stage 2
During the second stage, the progression of fatty liver disease can lead to more pronounced symptoms. Individuals may experience nausea, abdominal discomfort, bloating, and consistent fatigue without any clear reason. These symptoms are more evident during diagnostic imaging, as fat deposits within the liver tissue are more prevalent.
2.3 Symptoms in Stage 3
In the advanced stage of fatty liver disease, ultrasound and other imaging techniques often reveal a large increase in fatty tissue across the liver. This stage brings with it worsening symptoms such as upper right abdominal pain, jaundice, vascular lesions, severe fatigue, and accelerated weight loss. The appearance and worsening of these symptoms signal critical liver damage.

In stage 3, symptoms become pronounced, including right upper abdominal pain, loss of appetite, nausea, jaundice, and yellowing of the eyes.
3. Complications Associated with the Stages of Fatty Liver Disease
If left untreated, the advanced stages of fatty liver disease can lead to severe complications:
– Steatohepatitis (Fatty Liver Inflammation): Fat deposits around liver cells compromise liver function, inhibiting its ability to detoxify, which can lead to inflammation. This condition makes the liver more susceptible to infections and the toxic effects of viral agents.
– Cirrhosis: Over time, fat buildup causes liver cells to overwork, leading to fibrosis and scar tissue formation. Scarred areas progressively replace healthy liver tissue, disrupting normal function and rendering the liver unable to regenerate. Cirrhosis is irreversible, and advanced stages can lead to total liver failure.
– Liver Cancer: Prolonged fat accumulation often leads to cirrhosis, which is a primary risk factor for liver cancer. Cirrhosis from fatty liver disease is a silent yet serious progression that can lead to deadly outcomes without timely intervention.
4. Treatment Options for the Stages of Fatty Liver Disease
The stages of fatty liver disease offer windows of opportunity for intervention, especially in early detection cases. Treatments vary depending on the disease’s stage, with lifestyle adjustments proving most effective in the early stages. A balanced diet and regular exercise are critical first steps, especially for individuals at higher risk, such as those with obesity or diabetes.
In stages two and three, medical interventions may become necessary. Physicians may prescribe medications to reduce liver inflammation and control blood lipids. In cases of advanced fatty liver disease, close monitoring and lifestyle changes can help slow disease progression and alleviate symptoms.
5. Important Considerations for Managing Fatty Liver Disease
5.1 Weight Management
Weight loss remains an essential treatment for individuals with obesity-related fatty liver disease. A gradual approach to weight loss is crucial, as rapid weight reduction can worsen liver symptoms.
5.2 Vitamin E
Studies suggest that vitamin E can help reduce inflammation in individuals with non-diabetic fatty liver disease, though it is not suitable for everyone and must be taken under medical supervision.
5.3 Blood Lipid Control
Statins that bypass extensive liver metabolism may help manage blood lipid levels, helping reduce fat accumulation in the liver.
Regardless of the stages of fatty liver disease, maintaining a nutritious diet, engaging in moderate physical activity, and avoiding alcohol and harmful stimulants are essential. Recognizing the importance of early detection and following treatment recommendations can reduce the risk of complications and improve long-term health outcomes.

Liver elastography is an effective diagnostic method that assesses the degree of fat accumulation in the liver.
If you experience any symptoms consistent with fatty liver disease, consult a hepatology specialist for a thorough evaluation and personalized treatment plan. Early intervention remains the most effective way to manage and potentially reverse this progressive disease.








