Heart valve regurgitation is a common cardiovascular condition that directly affects the heart’s ability to pump blood efficiently. It occurs when one or more of the heart valves fail to close completely, allowing blood to flow backward instead of moving forward as it should. This backward flow decreases the heart’s pumping efficiency and, over time, can lead to heart failure and other serious complications. Recognizing the types, clinical manifestations, and treatment strategies for heart valve regurgitation is essential to managing the disease and improving long-term outcomes.
1. Overview of Heart Valve Regurgitation
1.1 Definition and Mechanism
Heart valve regurgitation refers to the improper closure of one or more heart valves during the cardiac cycle, leading to the backward flow of blood. The human heart has four valves: mitral, tricuspid, aortic, and pulmonary. When any of these valves becomes incompetent, it alters intrachamber pressures and increases the workload on the heart, potentially resulting in heart failure if left untreated.
The condition may be caused by age-related valve degeneration, congenital heart defects, rheumatic fever, infective endocarditis, or secondary to other heart diseases such as myocardial infarction or hypertension.
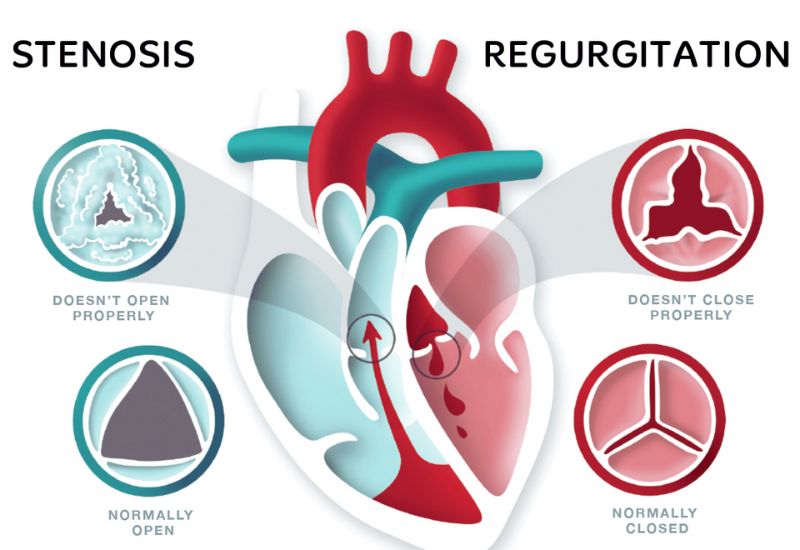
Heart valve regurgitation occurs when a valve fails to close completely during contraction, causing blood to flow backward.
1.2 Classification by Severity and Valve Location
Regurgitation is categorized by severity (mild, moderate, severe) and by the affected valve. Each type presents with distinct symptoms and requires tailored management.
Common types include:
– Mitral valve regurgitation – the most prevalent, affecting blood flow between the left atrium and left ventricle.
– Tricuspid valve regurgitation – involves the right atrium and right ventricle.
– Aortic valve regurgitation – backward flow from the aorta into the left ventricle.
– Pulmonary valve regurgitation – the least common, involving the right ventricle and pulmonary artery.
2. Major Forms of Heart Valve Regurgitation
2.1 Mitral Valve Regurgitation
This is the most frequently encountered form of heart valve regurgitation. The mitral valve lies between the left atrium and left ventricle, ensuring unidirectional blood flow. When it fails to seal properly, blood leaks backward into the atrium, causing pulmonary congestion and affecting breathing.
Typical symptoms include exertional shortness of breath, fatigue, palpitations, and leg swelling. In early stages, symptoms may be absent. Common causes include valve degeneration, rheumatic disease, annular dilation, or endocarditis.
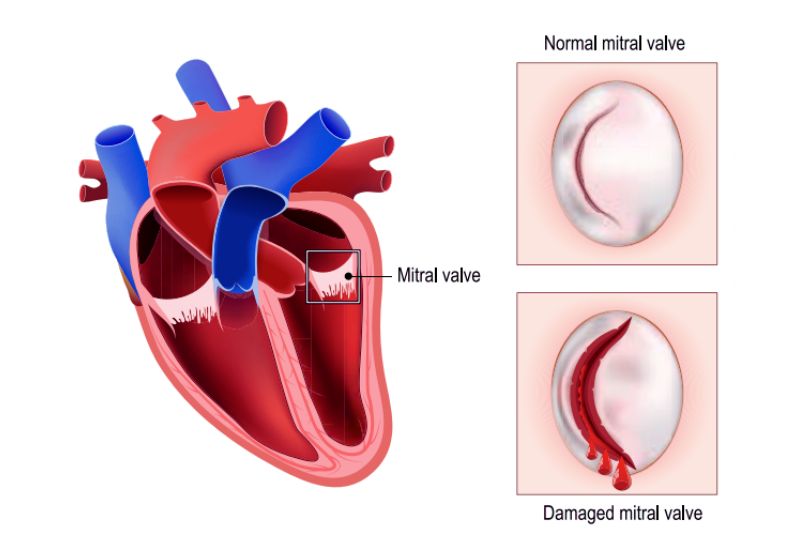
Mitral valve regurgitation is the most common type of heart valve disorder.
2.2 Tricuspid Valve Regurgitation
This occurs when blood flows backward from the right ventricle into the right atrium. Though less common, it often coexists with right heart disease or pulmonary hypertension. It raises systemic venous pressure, leading to peripheral edema, hepatomegaly, abdominal discomfort, and fatigue.
It may be congenital or secondary to structural valve damage. Treatment depends on the underlying cause and severity.
2.3 Aortic Valve Regurgitation
In this type, blood leaks from the aorta back into the left ventricle during diastole, causing the ventricle to enlarge and weaken over time. Symptoms include chest tightness, orthopnea (difficulty breathing when lying flat), fatigue, and dizziness due to reduced brain perfusion.
Common causes include aortic root dilation, rheumatoid disease, trauma, or endocarditis. This form of heart valve regurgitation often progresses rapidly and requires close monitoring.
2.4 Pulmonary Valve Regurgitation
The rarest form, often associated with pulmonary hypertension or repaired congenital heart defects like Tetralogy of Fallot. It may be asymptomatic initially but can lead to right ventricular dysfunction over time. Symptoms include mild chest discomfort, fatigue, and palpitations. Diagnosis typically relies on echocardiography and advanced imaging.
3. Clinical Signs and Potential Complications
3.1 Typical Symptoms
Patients may experience shortness of breath (especially during exertion or while lying down), chronic fatigue, palpitations, and peripheral edema. Cardiac murmurs are often detected during physical examination.
Symptom severity depends on the valve involved and the degree of regurgitation. Mild cases may remain unnoticed, while moderate to severe forms significantly affect quality of life and physical function.
3.2 Common Complications
Without timely diagnosis and treatment, heart valve regurgitation can result in:
– Heart failure
– Arrhythmias
– Thromboembolism
– Myocardial infarction
There is also a heightened risk of infective endocarditis, a life-threatening condition requiring immediate medical attention.
4. Diagnosis and Treatment
4.1 Diagnostic Methods
Diagnosis involves a combination of clinical evaluation and imaging techniques:
– Doppler echocardiography (primary tool)
– Electrocardiogram (ECG)
– Chest X-ray
– Cardiac MRI
– Cardiac catheterization (in selected cases)
Echocardiography plays a central role in assessing valve function, regurgitation severity, and guiding treatment decisions.

Treatment is tailored by cardiologists based on the valve involved, severity of regurgitation, and the patient’s overall health.
4.2 Medical Management
For mild to moderate heart valve regurgitation, medical therapy aims to control symptoms and reduce cardiac workload. Commonly prescribed medications include: Diuretics, vasodilator, beta-blockers, ACE inhibitors, antiarrhythmics.
Patients must undergo regular follow-ups to adjust treatment and monitor disease progression.
4.3 Surgical and Interventional Options
In advanced cases with significant symptoms or compromised heart function, valve repair or replacement is recommended. Minimally invasive techniques, such as transcatheter aortic valve implantation (TAVI), offer alternatives to open-heart surgery, though not without risk.
Treatment choice depends on valve location, patient health status, and expected outcomes, and must be determined by cardiovascular specialists.
4.4 Lifestyle and Long-term Monitoring
Lifestyle modification is vital. Patients should follow a low-sodium, heart-healthy diet, avoid smoking, engage in light exercise, and adhere strictly to prescribed medications. Regular follow-up visits and echocardiographic monitoring are essential for early detection of complications and assessing treatment effectiveness.
Heart valve regurgitation can be a silent yet serious condition with far-reaching consequences if neglected. A thorough understanding of its forms, symptoms, and treatment pathways empowers patients to manage their condition proactively. Early detection through routine health screening, combined with proper treatment and lifestyle adjustments, plays a pivotal role in preventing complications and enhancing quality of life.








