Coronary atherosclerosis poses a serious health risk and can be fatal at any time. Understanding the disease and its symptoms is crucial for early detection and effective management.
1. Understanding Coronary Atherosclerosis
Coronary arteries are blood vessels responsible for supplying blood to the heart. These arteries are lined by the endothelium, a thin layer of cells that facilitates smooth blood flow. However, the endothelium can be damaged by factors such as high fat and cholesterol levels, smoking, diabetes, and hypertension.
When the endothelium is damaged, plaques can form, leading to hardened arterial walls and narrowed arteries. These plaques consist of cholesterol, calcium, and other substances in the blood. Initially, these plaques might not significantly impact blood flow or heart function. Over time, however, they enlarge, further narrowing the arteries and reducing their elasticity. This decrease in blood and oxygen supply forces the heart to work harder, causing coronary atherosclerosis and potentially leading to severe complications.
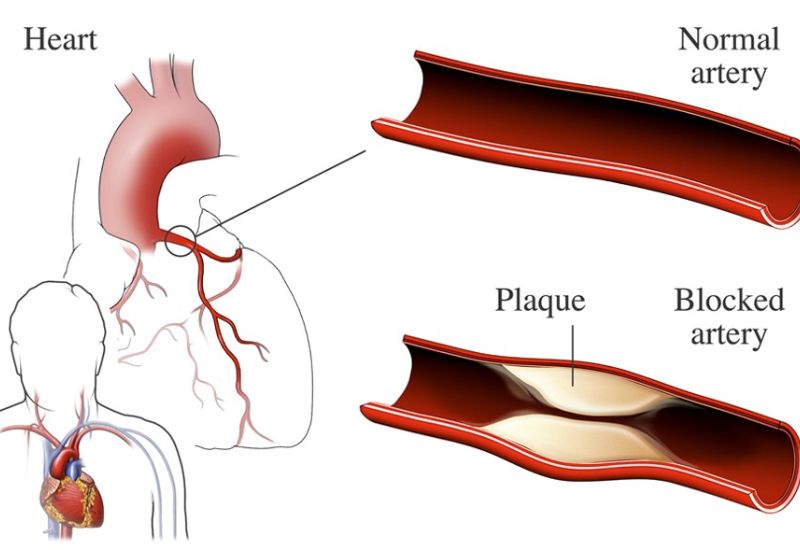
Coronary atherosclerosis develops due to the accumulation of plaques in the arterial walls.
2. Symptoms of Coronary Atherosclerosis
2.1 Angina That Eases with Rest
One common symptom is chest pain (angina) that subsides with rest. This pain often occurs during physical exertion, climbing stairs, playing sports, or experiencing psychological stress. It typically diminishes when the patient rests or takes vasodilators.
Symptoms include:
– Pain, discomfort, or pressure in the chest, beneath the breastbone
– Pain radiating to the jaw, neck, back, and arms
– Fatigue, shortness of breath, nausea
– Anxiety and stress
2.2 Sudden and Persistent Chest Pain
Patients may also experience sudden and persistent chest pain, even at rest, during stress, or due to weather changes, especially during the early morning hours. This pain can last over 15 minutes, not relieved by rest or vasodilators.
Plaque rupture is the main cause of this condition. Sudden and severe plaque rupture can completely block the artery, drastically reducing blood flow to the heart muscle and causing myocardial infarction (heart attack). Patients feel intense pressure or squeezing in the chest, with pain lasting a few minutes and recurring multiple times. Some heart attacks occur without chest pain, making early detection difficult.
3. Dangerous Complications of Coronary Atherosclerosis
3.1 Aneurysm
An aneurysm, one of the most severe complications, occurs when the artery wall weakens and bulges, forming a sac-like or fusiform shape that can rupture easily. This can lead to immediate death from severe blood loss, presenting symptoms like chest pain, shortness of breath, pale skin, and low blood pressure.
3.2 Stroke
Coronary atherosclerosis can also cause stroke, with blood clots blocking arteries and reducing blood flow to the brain. Mild cases may result in hemiplegia (paralysis on one side), while severe cases can be fatal.
3.3 Myocardial Infarction
Myocardial infarction results from ruptured plaques forming blood clots that obstruct blood flow, causing arrhythmias or cardiac arrest. After a heart attack, scar tissue forms, often leading to tachycardia (rapid heartbeat). About 90% of heart attack survivors develop this condition. Myocardial infarction is extremely dangerous, with one-third of patients dying before receiving treatment, and high recurrence rates within a year.

Coronary atherosclerosis can lead to myocardial infarction, a life-threatening condition if not treated promptly.
3.4 Heart Failure
Chronic heart failure occurs when the heart cannot pump enough blood to meet the body’s needs. Weakened heart muscles make pumping difficult, causing shortness of breath and fatigue.
4. Diagnosing Coronary Atherosclerosis
Diagnosis involves clinical symptoms and laboratory tests such as:
– Blood tests (in some cases)
– Electrocardiogram (ECG) to detect arrhythmias
– Echocardiogram to assess heart movement, left ventricular function, and valve diseases
– CT or MRI scans to accurately identify narrowed or blocked coronary arteries

MRI scans are currently the most accurate method for diagnosing coronary atherosclerosis.
5. Treatment Methods
Medications can improve coronary atherosclerosis, including:
– Cholesterol-lowering drugs (statins, fibrates)
– Anticoagulants (aspirin)
– Beta-blockers
– Diuretics for hypertension
– ACE inhibitors to prevent artery narrowing
These are common medications and should be prescribed by a doctor based on individual cases to avoid side effects. In severe cases, other treatments may be necessary to remove plaques and improve artery blockage.
Conclusion
Proactive health checks and lifestyle changes are vital for managing coronary atherosclerosis and preventing severe complications. Do not ignore unusual symptoms; early detection and timely treatment are key to effective management.








