Adenomatous colon polyps are a common issue, particularly for individuals over the age of 50. While not all colon polyps are dangerous, understanding their nature, detection methods, and treatments is crucial for maintaining good health.
1. What are Adenomatous Colon Polyps?
Adenomatous polyps, also known as adenomas, are a type of colon polyp and account for about two-thirds of all colon polyps. Although most adenomas do not become cancerous, they do have the potential to develop into colorectal cancer. The risk is assessed based on the polyps’ size, shape, and microscopic characteristics.
Generally, the larger the adenoma, the higher the chance it could become cancerous. Therefore, larger polyps, particularly those over 5 mm, should be completely removed to prevent them from progressing to cancer or significantly reduce the risk. After removal, polyp tissue samples are carefully examined under a microscope to determine their exact nature and evaluate cancer potential.

Colorectal adenomatous polyp images
2. Causes of Adenomatous Colon Polyps
2.1. Diet
Diet plays a significant role in the development of colon polyps. Diets high in fat and red meat and low in fiber can increase the risk. These factors can promote the formation of adenomatous polyps:
– Fat: Diets high in fats, especially saturated fats, can contribute to polyp formation by stimulating the growth of the colon’s mucosal cells, facilitating polyp development.
– Red Meat: Consuming large amounts of red meat, especially processed and grilled meats, can increase polyp risk. Red meat contains saturated fats and compounds that may damage the colon’s mucosa.
– Fiber: Fiber from fruits, vegetables, and whole grains is essential for a healthy diet. A lack of fiber can contribute to constipation and increase the risk of polyps. Fiber helps maintain colon health by providing nutrients to the mucosa and aiding in the elimination of harmful substances.
2.2. Smoking
Smoking can cause inflammation and damage to the colon’s mucosa, facilitating polyp development. Additionally, harmful substances in tobacco smoke can directly impact colon cells, causing genetic changes and abnormal cell growth, leading to polyp formation.
2.3. Obesity
Obesity is associated with an increased risk of polyps and colorectal cancer. Excess body fat, especially around the abdomen, can contribute to polyp development.
2.4. Aspirin and Non-Steroidal Anti-Inflammatory Drugs (NSAIDs)
Research suggests that using aspirin and NSAIDs can help reduce the risk of polyps and colorectal cancer. However, their use should be discussed with and monitored by a physician.
2.5. Age
Colorectal cancer and polyps are rare before age 40, with 90% of cases occurring after 50. Men are more commonly affected than women. Colorectal cancer screening is generally recommended starting at age 50 for both sexes.
2.6. Genetics
Family history and genetics play a crucial role in the development of polyps and colorectal cancer. Individuals with a family history of these conditions have a higher risk. Thus, colorectal cancer screening should begin earlier for those with a family history of polyps or colorectal cancer.

Family history and genetics are causes of adenomatous polyps.
2.7. Rare Genetic Disorders
Certain rare genetic disorders can increase the risk of colorectal cancer at a younger age than the general population. This is particularly relevant for families with a history of colorectal cancer. Genetic testing may be recommended to check for high-risk genetic mutations.
Understanding these causes helps individuals recognize the risks of adenomatous polyps and adopt appropriate preventive measures and screenings.
3. Diagnosing Adenomatous Colon Polyps
3.1. Colonoscopy
A colonoscopy is the most common and effective method for diagnosing colon polyps. This procedure involves using a flexible endoscope to examine the colon’s mucosa and remove any polyps. It allows doctors to see the entire colon surface and accurately identify existing polyps.
3.2. Fecal Occult Blood Test (FOBT)
Part of colorectal cancer screening includes testing for blood in the stool. Polyps can cause inflammation or bleeding in the colon’s mucosa, leading to detectable blood in the stool. A positive FOBT may prompt a colonoscopy to identify and locate polyps.
3.3. CT Colonography
CT colonography, or virtual colonoscopy, uses computed tomography to create detailed images of the colon. It provides an overview of the colon’s surface and can detect polyps. However, if polyps are found, a traditional colonoscopy is needed to remove them or determine their specific nature.
4. Removing Adenomatous Colon Polyps
4.1. Purpose of Polyp Removal
The primary goal of removing adenomatous polyps is to eliminate precancerous polyps that could develop into cancer if left untreated. Removing these polyps significantly reduces the risk of colorectal cancer.
4.2. Polyp Removal Methods
Polyp removal is performed through a colonoscopy. The doctor uses the endoscope to locate and remove the polyps. This process is painless since the colon’s mucosa lacks pain receptors.
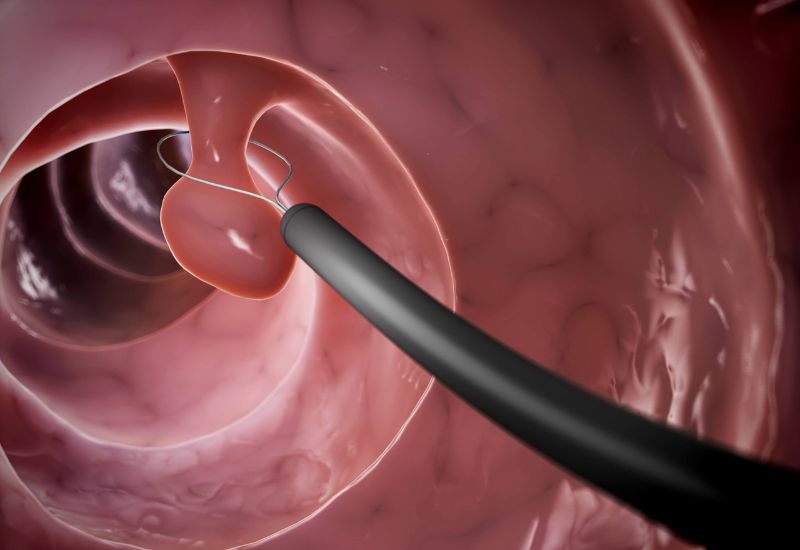
Removal of adenomatous polyps via colonoscopy.
4.3. Complications and Safety
Polyp removal is generally safe, though some risks and complications exist. The most common complications are bleeding and perforation (creating a hole in the colon). These occurrences are rare, with a low incidence rate (approximately 1 in 1,000 colonoscopies). Bleeding can be managed during the procedure using heat (electrocautery). Perforations sometimes require surgical repair.
By understanding the nature, causes, and treatment methods for adenomatous colon polyps, individuals can better protect their health and take necessary preventative measures.








